The Strategic Timing of Antiretroviral Treatment, or START study, is a clinical randomised controlled trial aimed at clarifying the optimal time to begin antiretroviral therapy for people living with HIV. The study sought asymptomatic, healthy individuals living with HIV with CD4+ T cells (an immune system health measure) above 500 cells per cubic millimetre (mm3). The primary objective was to determine if taking antiretroviral therapy immediately was superior to waiting until the CD4 cell count decline to 350 cells/mm3.
The START study, which was led by the International Network for Strategic Initiative in Global HIV Trials (INSIGHT), was conducted at 215 clinical research sites in 35 countries. Led by Principal Investigator James D. Neaton, Ph.D., of the University of Minnesota, the study enrolled 4,685 men and women living with HIV, aged between 18 to 81 years, with the mean age of participants being 36 years. Of these participants, 27% were female and approximately one-half of male participants identified as gay. All participants enrolled had a CD4 cell count above 500 cells/mm3, had no symptoms of the HIV infection, and had never taken antiretroviral therapy.
Participants of this international study were randomly assigned to either immediately commence antiretroviral treatment or delay treatment until their CD4 cell count dropped to 350 cells/mm3 or were diagnosed with an AIDS-defining illness. The antiretroviral drug regimen followed the pre-approved list of drugs based on the treatment guidelines of the U.S Department of Health and Human Services. Any subsequent changes to participant’s drug regimens were done in accordance with the antiretroviral treatment guidelines for that country.
Medical visit for the study participants were scheduled at one month, four months and for every four months following. Study participants were monitored for the development of AIDS, serious non-AIDS-related illness (such as cardiovascular disease events, end-stage kidney disease, liver disease and non-AIDS-defining cancers) and death from any cause. Participants were assessed to determine the risks and benefits of starting antiretroviral treatment early by outcomes such as adverse events, quality of life, hospitalisations, high-risk behaviours for transmitting HIV, and risk factors for serious non-AIDS conditions.
The first participant enrolled into the START study was in April 2009, with the study scheduled to finish in December 2016. However, on the 15 of May 2015, after a scheduled interim review of the study data by an independent data and safety monitoring board (DSMB), the START study was terminated ahead of schedule. The DSMB found strong evidence that there is significant benefit for starting antiretroviral treatment immediately before the CD4+ T-cell count drop from above 500 cells/mm3 to 350 cells/mm3. The following findings from the interim analysis ultimately influenced the DSMB recommendation to stop the START study:
- Reduction of risk of serious AIDS events, and deaths due to non-AIDS events, including cardiovascular events, renal and liver disease and cancer, by more than 50% amongst the early treatment arm when compared to the deferred arm
- Reduction on both serious AIDS and serious non-AIDS events, with greater effect on AIDS than non-AIDS events
- The two groups experienced similar safety outcomes (E.G. serious adverse event)
- Consistent findings were found across a number of pre-specified subgroups, including geographical regions
Furthermore, the DSMB recommended that all participants in the deferred treatment arm of the study, that had not begun therapy, would be offered immediate treatment. The study is still expected to conclude in late 2016 as all participants will be followed in the next stage of the study.
Professor Sean Emery, the co-ordinating investigator of the START study from the Kirby Institute at UNSW Australia hailed these results, saying “These findings have global implications for the treatment of people living with HIV”. These results have confirmed the belief that treatment at all stages of the virus extends the management of this chronic illness, preventing serious disease complications for those living with HIV. When combining the findings achieved from previous studies on the risk of HIV transmission among people on antiretroviral therapy, Professor Emery believes that the “these new findings support treatment for everyone with HIV”.
These findings are heartily welcomed by the WA AIDS Council because this study and its findings assists people diagnosed with HIV in navigating what can be an overwhelming decision when it comes to treatment. WA AIDS Council CEO Andrew Burry strongly believes that providing HIV positive individuals with clear evidence that informs and supports their choices empowers them to confidently make decisions that are best suited to their lives. With the availability of this new information, Burry feels that the anxiety and stress relating to the decision to commence treatment can be reduced. Liz Walker, the Positive Peer Educator at the Council agrees; “Australia has had unrestricted access to antiretroviral therapy for HIV-positive Medicare eligible individuals since April 2014, but the motivation to start treatment > 500 cells/mm3 was based on weaker observational data”. Walker believes that the findings from the START study will provide the world with gold standard evidence of the benefits of treating HIV infection early.
While the decision to treat HIV early is encouraged, the WA AIDS Council continues to support the belief that this decision is an individual one. In their work with people living with HIV, Walker encourages clients to make the best choices for their life and believes that HIV-positive individuals should discuss the START study with their HIV clinician. “For those who choose to defer antiretroviral treatment, it is important to remain part of the care system and continued monitoring and close follow-up with your clinician” says Walker.
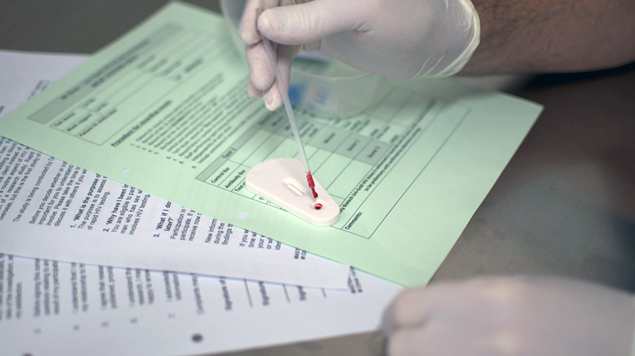
This conclusive evidence also strongly supports the importance of regular testing for those people vulnerable to HIV infection. As Burry asserts, “The benefits of early treatment depend on diagnosis. Regular and frequent testing means that treatment can begin much closer to the point of infection”. The WA AIDS Council advocates getting tested and testing more often at a clinical service experienced with HIV, such as the M Clinic or one of the sexual health clinics across WA.
Natalie Hadland
Western Australian AIDS Council
The M Clinic is a community sexual health clinic run by and for gay and other homosexually active men. To discuss your sexual health, you can call for an appointment (Phone: 9227 0734) and have a frank and open discussion with staff without any fear of judgement.
The information contained in this article does not constitute medical advice and is not intended to be a substitute for professional medical advice
SPONSORED





